For the millions living with chronic low back pain, the search for relief can feel like a frustrating, endless cycle of trial and error. In an age of personalized medicine, we assume the "right" treatment must be tailored to an individual’s specific symptoms and psychological state.
But what if a powerful therapy works for almost everyone?
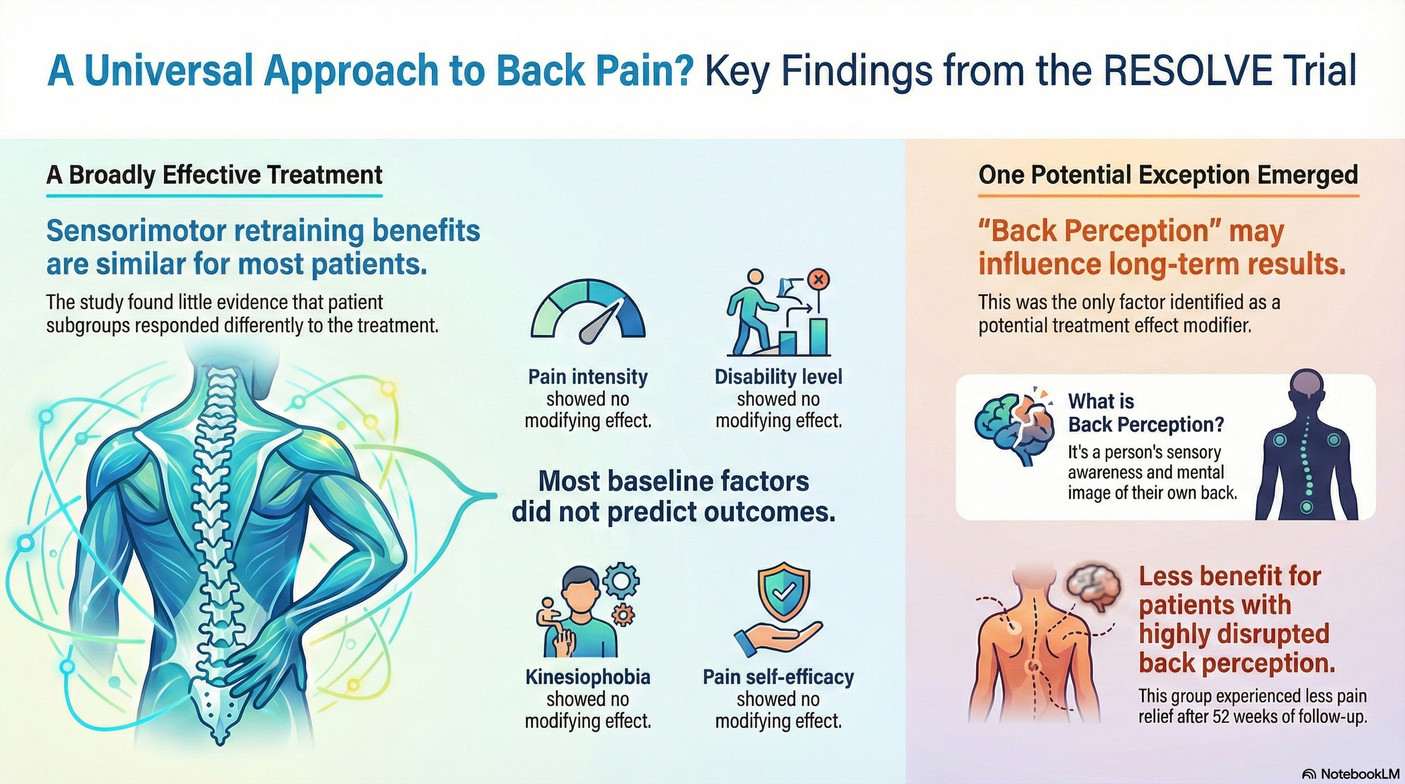
A major recent study, the RESOLVE trial, investigated a promising treatment called graded sensorimotor retraining, a rehabilitation package that consists of pain science education, premovement training, and graded movement and loading. Researchers conducted a deep analysis to see which types of patients benefited the most, and the results were surprisingly universal, challenging long-held ideas about who is a "good candidate" for recovery.
The Big Surprise: This Treatment Doesn't Play Favorites.
Going into the study, researchers had clear hypotheses. They expected that patients with the most severe symptoms—those with higher pain intensity, greater physical disability, or more intense fear of movement (kinesiophobia)—would actually benefit more from the therapy, as they had the most room for improvement.
But in a direct contradiction of these expert predictions, the study's main finding was clear: none of these factors significantly changed the treatment's effectiveness. Researchers rigorously tested whether eight baseline clinical and psychosocial characteristics predicted patient outcomes, and the results were consistently neutral.
This is a powerful and impactful discovery. It suggests that people can benefit from this therapy regardless of how severe their pain is or what their psychological state is when they begin. You don't have to wait to be the "perfect" patient to get better. The study's authors summarized this key finding:
These findings suggest that the benefits of graded sensorimotor retraining may be similar for all people with chronic low back pain, regardless of individual differences at baseline.
Your "Back Image" Matters, But Not How Experts Thought.
The analysis did find one factor that seemed to make a difference: "back perception." This is a person's mental image or awareness of their own back, an internal map that can become distorted or vague in people with chronic pain.
Again, the researchers' original hypothesis was straightforward: since the therapy is designed to restore this mind-body connection, they expected that people with a more disrupted back perception would benefit the most.
However, the study revealed the exact opposite. In the one statistically significant finding of its kind, the analysis found that people with a more disrupted back perception at the start of the trial actually experienced less benefit in terms of pain intensity after one year. This fascinating and counter-intuitive result suggests these individuals may have found it harder to engage with the exercises. The researchers note this surprising finding needs further study to be confirmed, but it opens up a new avenue for understanding who might need a modified approach.
What This Means for You: Hope is Universal, Not Exclusive.
For anyone with chronic back pain, these findings are overwhelmingly good news. They suggest that graded sensorimotor retraining is a broadly suitable and effective treatment for a wide range of people.
The message is empowering: you don't need to wait until you have the "perfect" mindset, lower your pain levels, or overcome your fears to start a treatment that could help. The therapy itself is designed to work on these very issues as part of the healing process.
This research allows clinicians to be more confident in recommending this approach to most patients with chronic nonspecific low back pain. At the same time, it highlights that they may need to provide extra support for those who have a highly disrupted perception of their back. The study's authors suggest this could include tangible strategies like "augmenting sensory feedback (eg, virtual reality or biofeedback), slowing task progression, or increasing premovement training."
A New Chapter in Treating Chronic Pain
In the modern quest for personalized pain treatment, the discovery of an intervention that is so universally effective is a major and hopeful step forward. The study shows that while every person's experience of pain is unique, the path to relief may be more accessible than we once thought.
As we continue to learn about the brain's profound role in pain, does the path to relief lie not in finding a unique key for every lock, but in discovering a master key that works for nearly everyone?