Summary
-
Pain is real and personal—it’s your nervous system’s alarm, shaped by body, brain, and context. (IASP)
-
Not all pain equals harm. Tissues can be safe while pain still “feels loud.” (IASP)
-
Movement helps most people. Graded activity and education show moderate evidence for easing long-standing pain. (Cochrane Library)
-
You don’t have to do it alone. Physical therapists can help you build a plan that fits your life and goals. (ChoosePT)
What it is (plain-language overview)
Pain is an unpleasant experience you feel in your body and interpret in your brain. It can show up with a clear injury (like an ankle sprain) or persist after tissues have healed. Today’s leading definition describes pain as an unpleasant sensory and emotional experience—meaning your biology, thoughts, mood, sleep, and stress can turn the “alarm” up or down. (IASP)
Clinicians often group pain by duration:
-
Acute: hours to weeks, usually linked to recent tissue stress or injury.
-
Subacute: weeks to three months.
-
Chronic (persistent): >3 months, sometimes without an ongoing injury. (NINDS)
Why it matters (symptoms, function, daily life)
Pain can limit walking, lifting, sleep, mood, focus, and social life. Many people begin to avoid activities, which can lead to deconditioning and even more pain during everyday tasks. The good news: with the right plan, most people can do more with less pain, even if some discomfort remains. Physical therapy focuses on function—getting you back to what matters at home, work, and in our Fayetteville–Manlius/Syracuse community. (ChoosePT)
How it works (simple physiology)
Think of your pain system as a smoke alarm:
-
Sensors in tissues detect potential threats (heat, pressure, chemical changes).
-
Signals travel via nerves to the spinal cord and brain.
-
The brain decides how loud the alarm should be, using context (stress, sleep, past experiences, and beliefs).
-
Over time, the alarm can become sensitized—it rings too easily or too loudly even when tissues are safe. Education, movement, and calming strategies can help recalibrate the system. (IASP, NINDS)
A quick comparison
| Type | Typical timeline | Common features | What often helps |
|---|---|---|---|
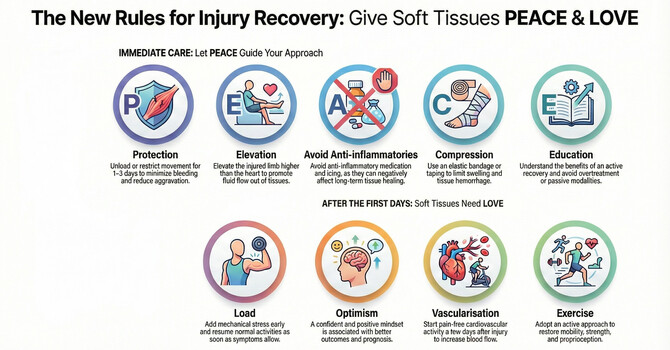
| Acute pain | Days–weeks | Clear cause, protective | Relative rest, gradual return to activity, short-term symptom relief |
| Persistent pain | >3 months | Alarm stays sensitive; activity avoidance is common | Graded exercise, education, sleep/stress support, pacing, consistent routine (Cochrane Library) |
| Flares | Hours–days | Temporary spike with stress, poor sleep, or overdoing | Dial down intensity/volume, active recovery, heat/ice as preferred, then resume plan |
What you can do today (practical steps)
-
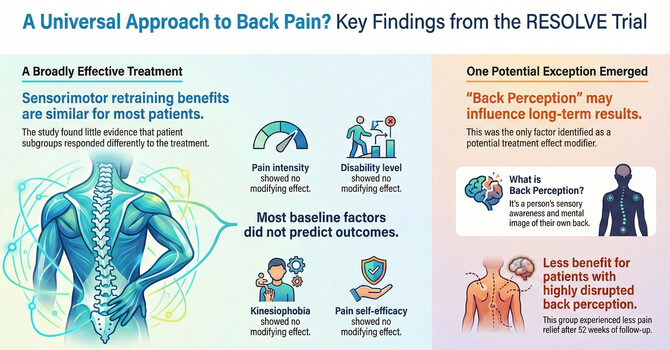
Keep moving—gently and consistently. Choose low-impact options you can repeat most days (walking, stationary cycling, water exercise, and light strengthening). Gradually increase one variable at a time (time, distance, or load). Moderate evidence supports exercise for persistent musculoskeletal pain. (Cochrane Library, PubMed)
-
Pace your day. Break tasks into smaller chunks with short “movement snacks” and rest breaks to avoid boom-bust cycles.
-
Sleep like it matters. Aim for a regular schedule, reduce screens before bed, and keep your room cool and dark. Poor sleep can amplify pain signals. (NINDS)
-
Practice a 1-minute calm reset. Try box breathing (inhale 4, hold 4, exhale 4, hold 4) a few times per day to lower system “threat.”
-
Use heat or cold—your preference. Short bouts can reduce stiffness or calm flares. Choose what feels best and doesn’t irritate your skin.
-
Stay social. Gentle activity with family or friends (a lap at Green Lakes or a neighborhood walk in Manlius) can lift mood and reduce pain’s impact.
-
Question unhelpful beliefs. “Pain = damage” is not always true; your alarm can be loud even when tissues are safe. Learning about pain can reduce fear and improve function. (IASP)
-
Partner with a professional. A PT can tailor exercise, pacing, and education to your goals, health history, and medications. The American College of Physicians guideline recommends non-drug options first for many back-pain cases. (American College of Physicians Journals, PubMed)
Safety notes: If you notice red-flag symptoms (new numbness/weakness, changes in bladder/bowel control, fever with back pain, unexplained weight loss, or sudden severe pain after trauma), seek prompt medical care. (NINDS)
When to see a physical therapist
Consider booking if:
-
Pain has lasted more than 2–3 weeks and limits walking, lifting, or sleep.
-
You’re having repeated flares that derail activity.
-
You’re returning to activity after illness, surgery, or a fall and want a safe plan.
-
You’ve grown fearful of movement and want guidance to restart.
-
You want a balance & mobility check to reduce fall risk and stay active in the Syracuse area.
Physical therapists are trained to evaluate, guide graded activity, and coordinate with your healthcare team. (ChoosePT)
Common myths → facts
-
Myth: “Pain always means damage.”
Fact: Pain warns of potential threat, but the alarm can be sensitive even when tissues are okay. Context matters. (IASP) -
Myth: “Rest until it’s 100% gone.”
Fact: Too much rest can prolong pain. Gentle, graded movement helps most people. (Cochrane Library) -
Myth: “Imaging will show the cause.”
Fact: Scans often show normal age-related changes that don’t match symptoms. Treatment focuses on function and goals, not pictures alone. (American College of Physicians Journals) -
Myth: “I’m too old to improve.”
Fact: Bodies adapt at any age. Progress may be slower, but strength, balance, and confidence can grow with the right plan. (ChoosePT)
Mini-FAQ
Is chronic pain “in my head”?
No. Pain is real. It’s produced by your nervous system and shaped by many factors—including tissue signals, stress, sleep, and beliefs. Addressing multiple factors helps. (IASP)
Should I avoid activities that hurt?
Short-term discomfort during graded activity can be okay if it settles within 24 hours and overall function is improving. A PT can help set safe boundaries. (ChoosePT)
Does exercise really help long-standing pain?
Yes—on average, exercise provides small-to-moderate benefits for pain and function, with few harms. The key is a program you can stick with. (Cochrane Library)
Heat or ice?
Either is fine—choose what feels best and use short bouts with a barrier on the skin. In general, it is recommended to use ice if you have an injury within 3 days.
When are medications appropriate?
For some conditions, short-term medicines can help, but many guidelines recommend starting with non-drug options like exercise and education. Discuss choices with your clinician. (PubMed)
Local next step
Live in Fayetteville–Manlius or the Syracuse area? Book a Basic Wellness Screening (15-minute check of balance & mobility) or a one-on-one consult at Unity Move Physical Therapy & Wellness. We’ll help you build a simple, confidence-building plan that fits your day.
References
-
International Association for the Study of Pain (IASP). Revised definition of pain. (IASP)
-
NINDS. Pain—overview and chronic pain definition. (NINDS)
-
Cochrane Review (Hayden et al., 2021). Exercise therapy for chronic low back pain—moderate-certainty evidence. (Cochrane Library, PubMed)
-
ACP Guideline (Qaseem et al., 2017). Noninvasive treatments for low back pain—start with non-drug options. (American College of Physicians Journals, PubMed)
-
APTA ChoosePT. Physical therapy and chronic pain—education and movement focus. (ChoosePT)