Stronger isn’t always better if the movement is poorly controlled. Motor control training teaches your brain and body to coordinate smoothly, so strength is used at the right time, in the right amount, in the right direction.
Think of traditional strengthening like putting a bigger engine in a car. Useful—but if the steering and alignment are off, you won’t drive better. Motor control is the steering, timing, balance, and precision. When you add strength on top of good control, your power transfers to real life: standing up, reaching, using stairs, turning, walking on uneven ground, and catching your balance after a slip.
Quick Takeaways
-
Motor control = how your nervous system plans, starts, and fine-tunes movement.
-
It often beats “strength-only” approaches for daily function because it improves timing, alignment, and balance.
-
At Unity Move PT, we personalize control training using a force plate, digital dynamometer, computer-vision motion capture, and surface EMG for real-time feedback and progress tracking.
-
Try today: a Tempo Sit-to-Stand (2-3-1): up for 2 seconds, down for 3, pause 1. Focus on smooth control, not speed.
-
Book a Movement Control Assessment to see your force, balance, and timing on screen in minutes.
What Is “Motor Control”?
Motor control is how your brain and body coordinate to produce smooth, safe, and efficient movement. It’s like cruise control + steering alignment for your body: you set a goal (stand up), your system chooses the right muscles, the right timing, and the right amount of force, then constantly adjusts to keep you steady.
Why Prioritize Motor Control Over Strength-Alone?
1) Efficiency
Better control means less wasted effort—movements feel smoother and more confident.
2) Joint Protection
Aligned movement spreads load across joints and tissues more evenly, reducing strain during daily tasks.
3) Balance & Falls
Good control improves weight-shift, righting reactions, and foot placement—key skills for walking outdoors at Green Lakes State Park, strolling Onondaga Lake Park trails, or navigating winter sidewalks. Exercise programs that target balance and functional movement reduce fall rates in older adults. (PubMed)
4) Pain Confidence
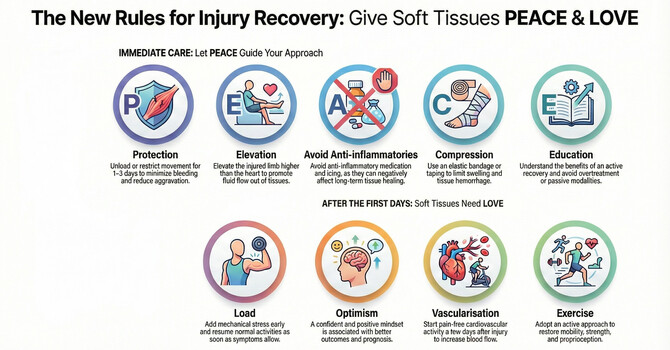
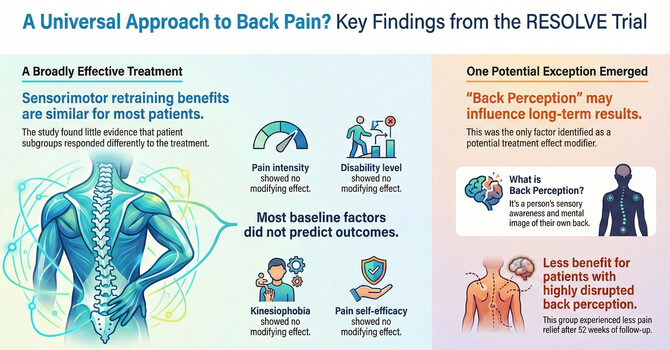
When your system learns timing and sequencing, muscles share the work better. This reduces “guarded” patterns and builds trust in movement. For low back pain, guidelines support exercise approaches that include specific trunk activation and motor control principles. (JOSPT)
Benefits of Motor Control Exercise By Condition
Musculoskeletal (MSK)
-
Low back, hip, knee, shoulder problems often involve timing and movement pattern issues.
-
Motor control work (e.g., trunk coordination, scapular control, hip-knee alignment) complements strength to improve function. (JOSPT)
Neuromuscular
-
In diabetic peripheral neuropathy and similar conditions, balance-focused exercise reduces fall risk and improves mobility. (PubMed)
Neurologic (Stroke, Parkinson’s)
-
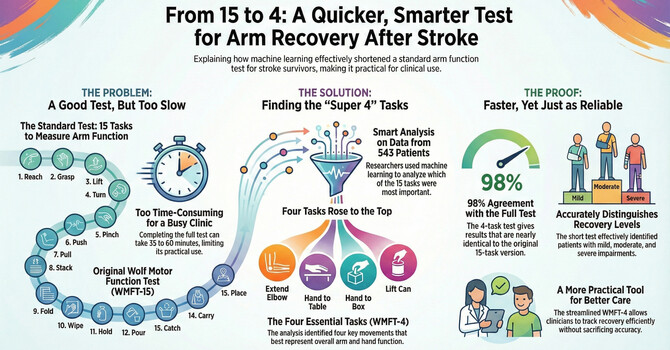
Task-specific, intensive practice (like repeated sit-to-stands and gait tasks) is recommended to rebuild walking and balance after stroke. (AHA Journals)
-
In Parkinson’s disease, physiotherapy guidelines emphasize cueing, gait/balance training, and task-specific practice to address freezing and slowness. (Parkinson's UK)
How We Personalize Motor Control at Unity Move (Tech is the Hero)
Force Plate
We measure balance, weight-shift symmetry, and rate of force development. This shows how you load each foot, how you step and land, and how you control sway. We then coach stance width, tempo, and foot-pressure cues based on your data.
Digital Dynamometer
Beyond “how strong,” we capture how you ramp force up and down—key for joint safety and everyday control (lifting groceries, standing from a chair). We train graded activation and smooth deceleration, not just max output.
Computer-Vision Motion Capture (Markerless)
Cameras estimate joint angles, timing, and asymmetry in real time. A cue like “knee over toes” becomes a measurable target with instant feedback. Research shows markerless systems are increasingly validated for clinical assessment and rehab applications. (BioMed Central)
Surface EMG (sEMG)
Small sensors display when muscles turn on/off and how much they work. This teaches sequencing (for example, glutes before low-back, tibialis before trunk sway)—exactly the kind of timing control people lose with pain or neurologic conditions. Meta-analyses suggest EMG biofeedback can improve limb function after stroke, particularly in the short term. (PLOS)
Bringing it together: We turn your assessments into simple dashboards and clear cues you can feel and see. You’ll watch your graphs change over time—great motivation and a concrete plan forward.
Motor Control Mini-Routine (10–15 Minutes)
Focus on tempo, timing, alignment, and “stopping power.” Use a sturdy chair and countertop. If anything feels sharp or unsafe, stop and call us.

1) Tempo Sit-to-Stand (2-3-1)
-
Purpose: Task control for daily standing.
-
Setup: Chair at knee height, feet hip-width, knees track over toes.
-
How: Lean slightly forward, up in 2 sec, down in 3 sec, pause 1 sec just above the seat.
-
Dosage: 2–3 sets × 6–8 reps; rest 30–60 sec.
-
Progress: Cross arms; slower tempo; add a small pause at mid-way.
-
Regress: Higher seat; use hands lightly.
-
Safety: Keep knees aligned; breathe steadily.
2) Tandem Balance with Head Turns
-
Purpose: Visual–vestibular control and weight-shift.
-
Setup: One foot directly in front of the other; counter nearby.
-
How: Hold tall posture, turn head left-right slowly while keeping a steady gaze target.
-
Dosage: 3 × 20–30 seconds per stance; switch feet.
-
Progress: Narrow stance; close eyes briefly (with support nearby).
-
Regress: Wider stance; reduce head movement.
-
Safety: Light fingertip support as needed.
3) Step-and-Pause Weight Shift
-
Purpose: Rhythm and stance time for walking.
-
Setup: Stand tall, step forward a short distance.
-
How: Step → pause 1 sec with weight on the front foot; push back to start.
-
Dosage: 2–3 sets × 8–10 steps/side.
-
Progress: Longer pause; add a small heel raise on the front foot.
-
Regress: Smaller step; hold support.
-
Safety: Clear the floor; move slowly.
4) Wall Slide + Lift-Off
-
Purpose: Scapular control for reaching.
-
Setup: Forearms on wall, elbows below shoulders.
-
How: Slide up in 2 sec, feel shoulder blades up + out, then a gentle lift-off for 1 sec without shrugging; return in 3 sec.
-
Dosage: 2 sets × 8–10 reps.
-
Progress: Add a light band; slower tempo.
-
Regress: Smaller range.
-
Safety: Keep neck relaxed.
5) Heel-Tap to Target
-
Purpose: Hip-knee control without knee collapse (valgus).
-
Setup: Stand on one leg, tap the opposite heel to a tape mark.
-
How: Soft knee on the stance leg; tap-return in control.
-
Dosage: 2 sets × 6–8 taps/side.
-
Progress: Farther target; slower return.
-
Regress: Use light hand support; closer target.
-
Safety: Stop if knee caves in; focus on tripod foot.
Common Mistakes & Quick Fixes
-
Holding breath → “Smell the rose, blow the candle.”
-
Rushing reps → Use a metronome or count out loud (2-up/3-down/1-pause).
-
Collapsing arches → “Tripod foot”: big toe, little toe, heel share the load.
-
Over-gripping → “Soft hands—let your legs and hips do the work.”
-
Eyes down → “Eyes on the horizon” for balance tasks.
Build the Habit (2-Week Starter Plan)
-
Frequency: 3 days/week
-
Time: 10–15 minutes
-
Track: One simple metric (e.g., tandem balance time or sit-to-stand tempo quality).
-
Week 1: Learn the cues and tempos; shorter sets if needed.
-
Week 2: Add one progression (slower tempo, smaller base of support, or longer pause).
-
Tip: Pair your routine with a daily habit (after morning coffee or evening TV) to make it stick.
When to Get Help
-
Red flags: Sudden severe pain, new numbness/weakness, unexplained dizziness, or falls—call your clinician.
-
Why an assessment helps: If your movement is asymmetric, poorly timed, or guarded, we’ll measure it and target the key limiter.
-
Our edge: Force plate + dynamometer + motion capture + sEMG let us see what the eye can’t and coach the exact cue that changes your movement today. Stroke and Parkinson’s programs benefit from task-specific practice—we quantify and progress it. (AHA Journals)
FAQ
Isn’t strength enough?
Strength matters, but without timing and alignment you won’t move better—or feel safer. Guidelines support exercise approaches that include specific activation/motor control for common problems like low back pain. (JOSPT)
Will I sweat?
Maybe a little. Control training is about precision, tempo, and balance, not heavy loads.
How soon will I feel steadier?
Many people notice smoother, more confident movement within 2–4 weeks of regular practice, especially when feedback tools guide the right cues.
Do I need equipment?
No. A chair and countertop are enough to start. Our clinic tools personalize your plan and track progress.
Can I do this with knee or shoulder pain?
Yes—movements are modifiable. We’ll adjust range, stance, tempo, and support so you train control within comfort.
How do your tech tools help me?
They show what’s really happening—how you load each foot, how fast you ramp force, how your joints align, and how your muscles fire—so coaching is precise. Early studies support these tools for rehab assessment and biofeedback. (BioMed Central)
One-Week Action Plan (Control > Load)
-
Day 1: Movement Check at Unity Move (15 min) or perform the Tempo Sit-to-Stand + Tandem Balance at home.
-
Day 2: Walk outdoors (level path) and practice step-and-pause every 5th step.
-
Day 3: Repeat the mini-routine; note any smoother reps or longer balance time.
-
Day 4: Light walk at Green Lakes or a mall; focus on quiet footfalls.
-
Day 5: Mini-routine with one progression (slower tempo or longer pause).
-
Day 6: Rest or gentle mobility.
-
Day 7: Re-test your best tandem balance time and write down your win.
References
-
Cochrane Review—Falls Prevention (2020): Exercise programs targeting balance/functional tasks reduce fall rates in community-dwelling older adults. (PubMed)
-
JOSPT Low Back Pain CPG (2021): Recommends exercise approaches including specific trunk activation/motor control for LBP. (JOSPT)
-
Cochrane/Expert Review—Motor Control Exercise for Chronic LBP (2016): MCE improves pain vs minimal care and performs similarly to other exercise approaches. (PubMed)
-
AHA/ASA Stroke Rehab Guideline (2016) & summary (2021): Endorses intensive, task-specific mobility and gait training after stroke. (AHA Journals)
-
European Physiotherapy Guideline for Parkinson’s (reviewed 2022): Supports targeted physiotherapy for gait, balance, and mobility across disease stages. (Parkinson's UK)
-
sEMG Biofeedback Meta-analysis (2024): EMG biofeedback can improve upper/lower limb function post-stroke, especially short term. (PLOS)
-
Markerless Motion Capture Review (2023): Growing validity and clinical applications for assessment and rehab. (BioMed Central)
Call to Action
Book a Movement Control Assessment at Unity Move—see your force, balance, and timing on screen in minutes.
Call 315-687-8678 or visit unitymovept.com.